CASE REPORT
A 53-year-old lady presented with bilateral mid-peripheral RPE disturbance and macular drusen. She had nyctalopia that predated bilateral refractive surgery performed 7 years earlier.

Examination elsewhere, 18 years previously, had revealed ‘craters at the back of the eye’, which had not been followed up. She took vitamins and fish oil and had never smoked.
There was a strong family history of ‘poor vision’, diagnosed as AMD, which had an early age of onset; her brother developed severe visual loss at age 53, her father at age 45, and her paternal grandfather and possibly great-grandfather had poor vision. All these men were smokers.
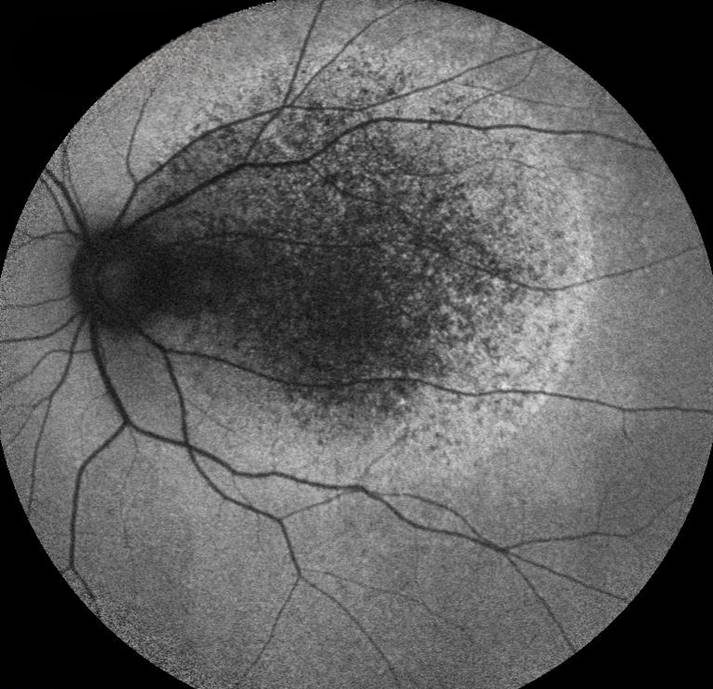
At presentation, her visual acuity was 6/6 bilaterally. Smartphone Fundoscopy revealed widespread pale deposits in both retinae and diffuse pigment changes in both maculae. Fluorescein fundus angiography revealed the typical Sorsby Fundus Dystrophy feature of patchy slow choroidal filling in the macula but no CNVM.
Based on the presentation, she was diagnosed with Sorsby Fundus Dystrophy.
DISEASE
Sorsby Fundus Dystrophy, also known as Sorsby Macular Dystrophy, is a rare progressive autosomal dominant macular dystrophy, presenting between the third and sixth decades of life.
First described in 1949, it is typically characterized by retinal atrophy and retinal detachment leading to a loss of central vision, then peripheral vision, and eventually blindness. Although a clear prevalence of Sorsby Fundus Dystrophy has not been characterized, estimates predict its occurrence to be 1 in 220,000.

Common pathologic characteristics include thick drusen-like deposits between the inner collagenous layer of Bruch’s membrane and the basement membrane of the retinal pigment epithelium (RPE).
Its underlying pathophysiology consists of an autosomal dominant mutation in the tissue inhibitor of the metalloproteinase-3 gene (TIMP3), due to which dysregulated TIMP3 proteins form deposits in Bruch’s membrane.
Common symptoms include progressive vision loss, sudden loss in visual acuity, or nyctalopia. Slit lamp examination may reflect drusen deposition in the posterior pole and along vascular arcades, reticular drusen, and progressive choroidal neovascular membranes.
Although there are currently no effective treatment options, anti-VEGF treatment has shown clinical efficacy in treating secondary choroidal vascular membrane formation (SCVM).
MANAGEMENT
Medical therapy
Sorsby Fundus Dystrophy and its associated TIMP-3 mutations do not have an effective or definitive treatment regimen yet. Prior medical therapies for Sorsby Fundus Dystrophy included vitamin A, thermal photocoagulation, and photodynamic therapy (PDT) with verteporfin; however, all treatment modalities showed low efficacy with some development of adverse effects.
Vitamin A was hypothesized to combat nyctalopia, but low doses were not effective, while high doses provoked noxious liver injury. Thermal photocoagulation was initially utilized to combat choroidal neovascular membrane (CNV) formation but did not lead to clinical improvement and paradoxically worsened membrane formation.
PDT verteporfin was either utilized as monotherapy or in conjunction with corticosteroid injections, but due to reduced clinical efficacy, was stopped.
Anti-vascular endothelial growth factor (anti-VEGF) treatment has shown clinical efficacy in treating secondary choroidal vascular membrane formation (SCVM). One systematic review compiled 14 studies with a total of 31 Sorsby Fundus Dystrophy patients and found that 51% of eyes with Sorsby Fundus Dystrophy maintained a log mar visual acuity of 0.5 if assicuated SCVM was treated early.
Treatment with an anti-VEGF regimen found 67% of these eyes with SCVM were able to remain functional with a visual acuity of 0.2 or better.
However, the limited utility was noted if patients presented with disciform scarring prior to treatment. Additionally, treatment with an anti-VEGF regimen did not protect patients from further macular scar formation, and 5-year follow-up of these patients did in visual acuity (the overall follow-up time for the patients in this review was 54 months).
Various studies have reinforced the efficacy of an anti-VEGF regimen in Sorsby Fundus Dystrophy patients, but do not specify a scheduled regimen. While certain studies advocate for treatment and extended protocol, others were not predisposed toward one approach.
A single report on Sorsby Fundus Dystrophy has also detailed the use of triamcinolone injections and adalimumab in the use of preserving vision.

Given the low prevalence of patients with Sorsby Fundus Dystrophy and the lack of effective treatment regimens, it is vital to host patient-centered discussions with the patient’s interests at the forefront. Various approaches may be time-intensive, ineffective, or cost-prohibitive; these should be taken into consideration before potential treatment.
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- SORSBY A, MASON ME. A fundus dystrophy with unusual features. Br J Ophthalmol. 1949 Feb;33(2):67-97. doi: 10.1136/bjo.33.2.67. PMID: 18111349; PMCID: PMC510908.
- Christensen DRG, Brown FE, Cree AJ, Ratnayaka JA, Lotery AJ. Sorsby fundus dystrophy – A review of pathology and disease mechanisms. Exp Eye Res. 2017 Dec;165:35-46. doi: 10.1016/j.exer.2017.08.014. Epub 2017 Aug 26. PMID: 28847738.
- Polkinghorne PJ, Capon MR, Berninger T, Lyness AL, Sehmi K, Bird AC. Sorsby’s fundus dystrophy. A clinical study. Ophthalmology. 1989 Dec;96(12):1763-8. doi: 10.1016/s0161- 6420(89)32654-6. PMID: 2622621.
- Fariss RN, Apte SS, Luthert PJ, Bird AC, Milam AH. Accumulation of tissue inhibitor of metalloproteinases-3 in human eyes with Sorsby’s fundus dystrophy or retinitis pigmentosa. Br J Ophthalmol. 1998 Nov;82(11):1329-34. doi: 10.1136/bjo.82.11.1329. PMID: 9924344; PMCID: PMC1722431.
- Gliem M, Müller PL, Mangold E, Bolz HJ, Stöhr H, Weber BH, Holz FG, Charbel Issa P. Reticular Pseudodrusen in Sorsby Fundus Dystrophy. Ophthalmology. 2015 Aug;122(8):1555-62. doi: 10.1016/j.ophtha.2015.04.035. Epub 2015 Jun 12. PMID: 26077580.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE

