CASE REPORT
A 37-year-old male, presented to an ophthalmology clinic with complaints of visual disturbances and ocular discomfort. He reported experiencing blurred vision, redness, and occasional pain in his left eye over the past few weeks.

There was no history of trauma or significant past ocular complaints. He mentioned that he had undergone multiple surgeries for intestinal polyps in the past.
On examination, His best-corrected visual acuity was 20/20 in the right eye and 20/40 in the left eye. External examination revealed mild eyelid erythema.
Intraocular pressure was within normal limits bilaterally. Anterior segment examination of the left eye revealed mild corneal edema and cells in the anterior chamber. The right eye examination was unremarkable.
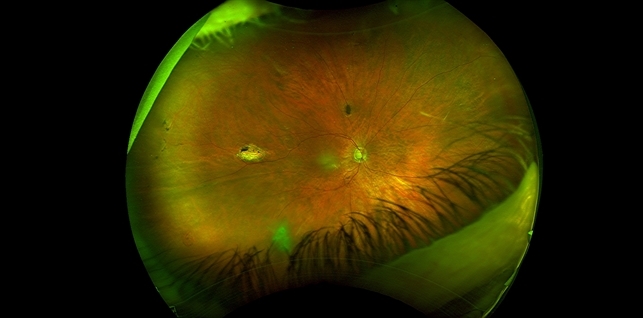
Dilated fundus examination revealed the presence of multiple pigmented retinal lesions in both eyes. These lesions appeared as well-demarcated, flat, and hyperpigmented patches distributed throughout the peripheral retina.
Some lesions exhibited a characteristic “Gardner sign,” showing bony spicules extending into the retina (salt-and-pepper appearance). No retinal detachments or vitreous abnormalities were noted.
Based on the clinical findings, ocular manifestations were consistent with Gardner syndrome.
DISEASE
Gardner syndrome is a rare phenotypic variant of familial adenomatous polyposis (FAP). Both Gardner syndrome and FAP are characterized by the numerous adenomatous polyps lining the intestinal mucosal surface.

However, Gardner syndrome has characteristic polyps in the colon and osteomas that help distinguish the disease from FAP. Gardner syndrome can also present with ocular manifestations that include the presence of multiple patches of congenital hypertrophy of the retinal pigment epithelium (CHRPE).
The presence of multiple and bilateral CHRPE is considered a clinical disease marker and is useful for early detection in individuals that are at risk. However, the absence of CHRPE cannot be considered a negative predictive indicator of Gardner syndrome.
The earliest and most common extra-colonic finding in Gardner syndrome is CHRPE which is found in nearly 90% of patients. However, ocular findings in Gardner Syndrome are often incidental so family history is the most critical assessment of a patient’s risk.
Since Gardner syndrome is an autosomal dominant disorder, the offspring of an affected parent pose a 50% chance of inheriting the disease. Less commonly, with no known causes, Gardner syndrome can result from de novo mutations in the APC gene.
De novo mutations account for approximately 20% of individuals diagnosed with Gardner syndrome and have an absent family history.
MANAGEMENT
General Treatment
Eye Abnormalities
Active intervention is not generally indicated or required. In rare cases, proton beam therapy has been indicated.
Systemic Abnormalities
Once individuals become aware of familial inheritance or are diagnosed with Gardner syndrome, treatment is aimed at the prevention of polyp growth in the colon. Treatment often includes the use of sulindac or celecoxib.
Sulindac is an NSAID and celecoxib is a COX2 inhibitor which both aid in decreasing polyps growth. If the disease progresses and more than 20 polyps are present then removal of the colon is recommended.
Complications and Prognosis
Currently, there is no cure for Gardner syndrome. If surgery is not performed or polyp growth is not controlled, patients will inevitably develop colon cancer by the age of 40. As of now, management and surveillance of symptoms are first-line treatments.
Surveillance includes annual physical exams to monitor thyroid function, palpate the liver, assess liver function, and abdominal ultrasound. Beginning at ages 20-25 abdominal CT should be assessed every 3 years along with monitoring the adrenal glands, small bowels, and pancreas.
Would you have interest in taking retina images by smartphone?
Fundus photography is superior to fundus analysis as it enables intraocular pathologies to be photo-captured and encrypted information to be shared with colleagues and patients.
Recent technologies allow smartphone-based attachments and integrated lens adaptors to transform the smartphone into a portable fundus camera and Retinal imaging by smartphone.
RETINAL IMAGING BY YOUR SMARTPHONE
REFERENCES
- Charifa A, Jamil RT, Zhang X. Gardner Syndrome. [Updated 2021 Jun 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482342/
- Juhn E, Khachemoune A. Gardner syndrome: skin manifestations, differential diagnosis and management. Am J Clin Dermatol. 2010;11(2):117-22. doi: 10.2165/11311180-000000000-00000. PMID: 20141232.
- Laghmari M, Lezrek O. Congenital hypertrophy of the retinal pigment epithelium in Gardner’s syndrome. The Pan African medical journal. 2014;19:164. doi:10.11604/pamj.2014.19.164.4518
- Lewis RA( 1 ), Crowder WE( 2 ), Nussbaum RL( 2 ), Eierman LA( 3 ), Ferrell RE( 4 ). The Gardner Syndrome: Significance of Ocular Features. Ophthalmology. 91(8):916-925. doi:10.1016/S0161-6420(84)34213-0
- Giardiello FM, Brensinger JD, Peterson GM. AGA technical review on hereditary colorectal cancer and genetic testing. Gastroenterology 2001; 121: 198-213.
- Pinto RS, Simons A, Verma R, Bateman N. Gardener-associated fibroma: an unusual cause of upper airway obstruction. BMJ Case Rep. 2018 Sep 28;2018.
RETINAL IMAGING BY YOUR SMARTPHONE

RETINAL IMAGING BY YOUR SMARTPHONE


Please provide me with more details on the topic